3. Role of e-Health standards in the life cycle of specifications and data in healthcare
Standards are specifications for repeated use which are used for setting requirements and providing existing models for products, systems, or services. e-Health standards are used in many different phases of solution development for health and social care information systems (see Figure 1). These systems and solutions are acquired, deployed, and used in various health care settings for clinical and administrative purposes. Systems and solutions are also used for further data collection and many different secondary use purposes such as population health management, organizational management, and research. Testing conformance to specifications may be performed before acquisitions.
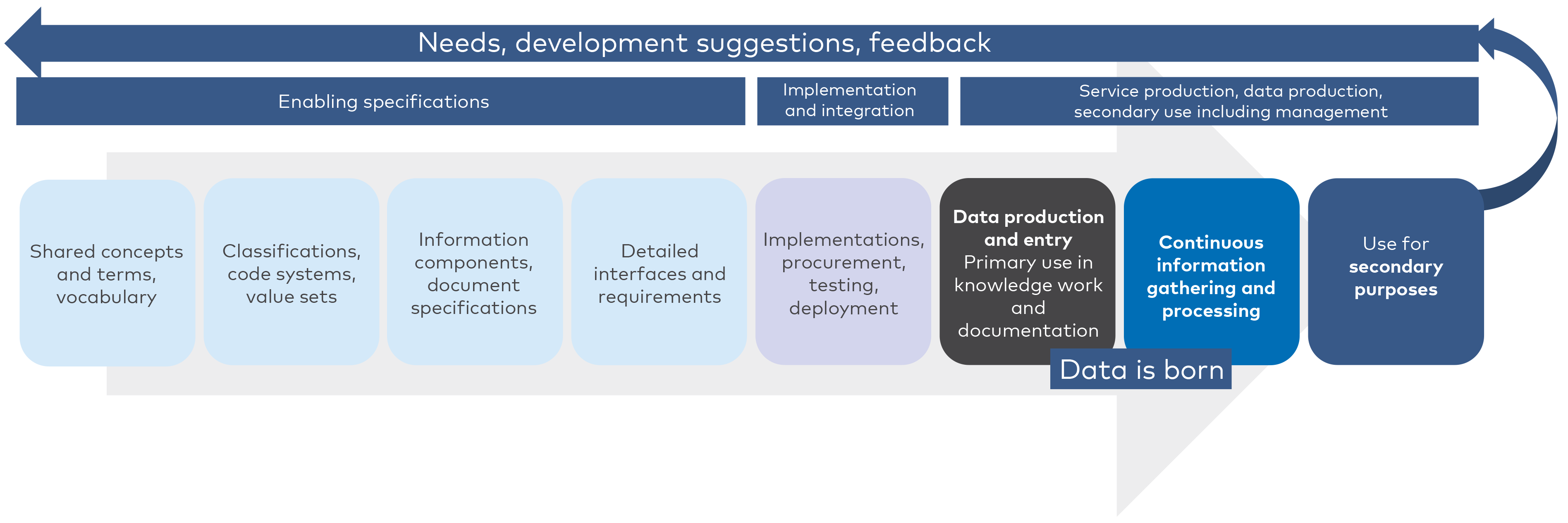
Figure 1. Specifications are the basis for implementation of ICT and EHR systems used in production of health services, as well as data entry, information gathering and data reuse.
It must be noted that the life cycle of data begins from use of systems which have already been built and acquired. e-Health standards and specifications are used in an earlier phase for enabling systems implementation and creation of data. Creation of data or data entry takes place in documentation of health care work or for specific information gathering purposes. Thus, enabling specifications such as e-Health standards have an effect to the features of systems and solutions, as well as data quality.
There are various aspects of ICT solutions in healthcare which are supported by e-Health standards.
e-Health standards that support semantic interoperability include information models and conceptual models, code systems and terminologies, as well as supporting data types. These are utilised in interfaces, structured documents, and systems to give structure and context to data. Standards are implemented in systems which are used to create, process and transfer data. Many e-Health standards for electronic health records deal with these aspects of interoperability. Semantic e-Health standards for terminology, classifications and code systems can be an enabler for shared understanding of concepts as well as content in information which is to be exchanged and reused. A shared understanding between different users has traditionally been perceived as crucial. However, computable semantic interoperability which supports automation and artificial intelligence has been increasingly proposed in recent years.
The emphasis on more and more structured information has been partially driven by classification and automation needs or documentation responsibilities which are not always directly related to immediate needs of health professionals at the point of care. A risk of over-structuring of non-relevant information or requiring information which is perceived to bring little value to the immediate work of professionals has been identified.
In addition to information standards, e-Health standards are available for functional requirements of systems. Use of these standards gives standardized vocabulary and common preconditions for requirements specifications in systems acquisitions by health service provider organisations. Such standards can also be used to provide a clear division of work between subsystems or applications from different vendors. These standards can also be used to refine the scope of requirements to be harmonised across EHR systems in regulation.
Standards are also available for many security aspects of systems, identification of systems and actors, as well as reference e-Health standards for systems architectures and process modelling.
Open and web-based technologies such as XML and JSON are widely used for domain-specific e-Health standards in healthcare.
Many interoperability standards focus on information exchange between systems and shared information models or terminologies. However, there are also user interface-oriented standards which aim to improve usability of systems, to support single sign-on and to ease navigation between distinct systems or modules, even without directly sharing or exchanging data.
There are also standards initiatives to support uniform presentation of graphical symbols and visual user interface layouts for health information systems. Use of standard terms and glossaries also supports uniform representation in user interfaces which may improve efficiency and usability of systems use.
However, semantic, and technical interoperability between systems and organisations has been the main driver for eHealth standardization. These e-Health standards also support standardized guidelines and knowledge models for healthcare.
Many international standards need further refinement for more specific use cases. This refinement may take place in standards development organizations (on both an international and national level), national authorities, or it may be performed by vendors, just to name a few actors who refine or profile standards.
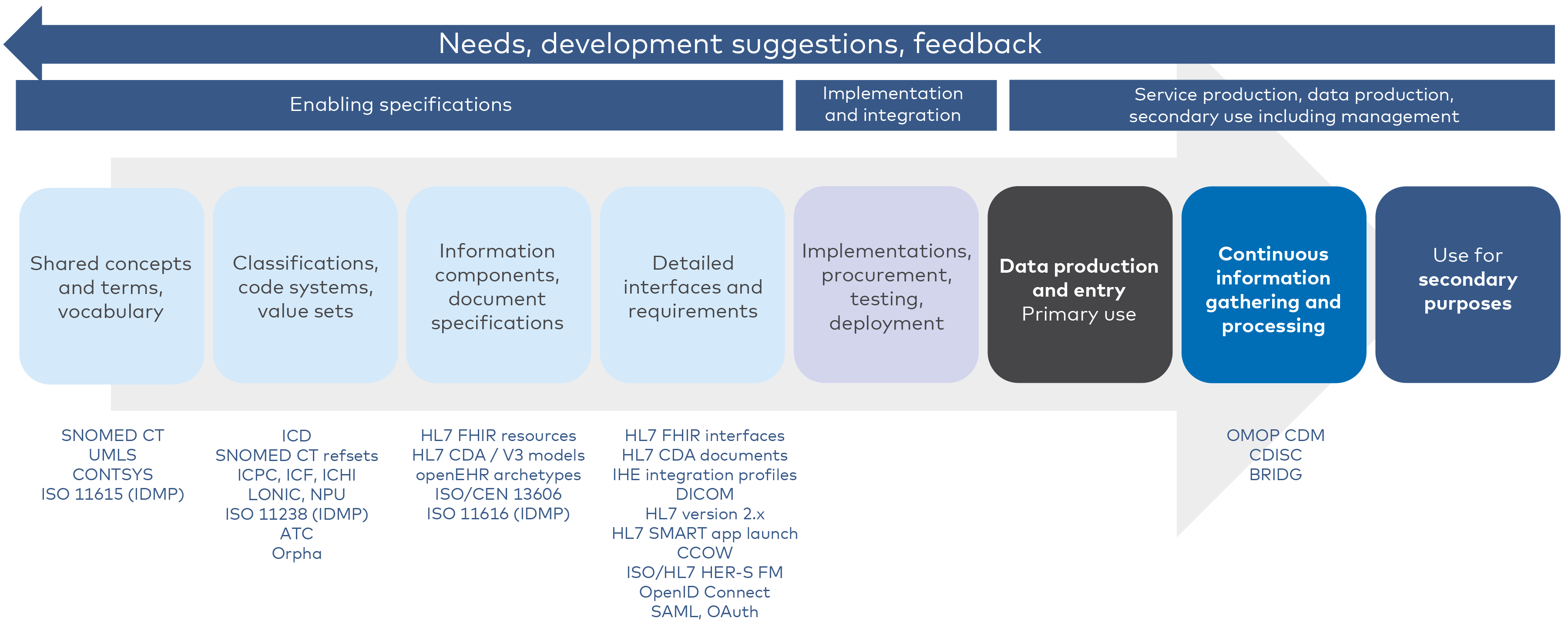
Figure 2. Examples of standards supporting different phases of the life cycle (this is not an exhaustive list of standards)
Standardization processes have built-in features for balancing and involving different and – sometimes – even competing interests and groups. The built-in openness and transparency in standardization processes promote trust between different stakeholders.
e-Health standards as enabling specifications, are often not directly visible to users of the systems or data. Despite their relative invisibility however, e-Health standards thoroughly influence many features of the systems and many aspects of data. At its best, a standard promotes high quality of information systems used by professionals and promotes high data quality. Features of the standard may support the daily work of professionals without the standard being visible to the users of the system. Conversely, problems in the content or application of standards, or problems in some of the requirements of the standards may hinder usability, efficiency, or other aspects of systems. This may further be reflected as problems in data production and may adversely impact user satisfaction, data quality and the daily work of users.
The diligent use of standards in early phases of the overall life cycle of systems should reduce the need for data harmonization and correction in later phases of the life cycle. Knosp (2020) summarizes this well: “Effective data interoperability leads to improved efficiency of methods and processes, improved time from research project design, through trend identification to policy implementation”.
In this guideline, we mainly focus on interoperability standards and exclude standards which deal with technical and security aspects, software development processes and generic quality systems.